When it comes to uterine health, many women have heard of endometriosis. It’s a common condition, and for some women can be debilitating during menstruation. Many of us know someone who suffers from ‘endo’ and understands the impact it can have on their daily life.
But there is a similar condition that is less well-known - adenomyosis. Another condition affecting the uterus, it presents similar symptoms as endometriosis and can be caused by similar issues. Treatment options are also similar.
To complicate things further, fibroids grow in the uterus again presenting similar symptoms.
So why do we need to discuss the conditions and compare them?
It all comes down to the uterine tissue and where it grows.
In this blog we'll cover the major differences between endometriosis, adenomyosis, and uterine fibroids by looking at the symptoms, causes, diagnosis methods and treatment options available.
Inside Vs Outside
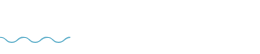
A common method of discussing the difference between endometriosis and adenomyosis is ‘inside vs outside’.
Endometriosis is a condition where tissue that should be on the inside of the uterus grows on the outside. Adenomyosis sees uterine tissue growing deeper than it should.
Endometriosis = outside.
Adenomyosis = inside.
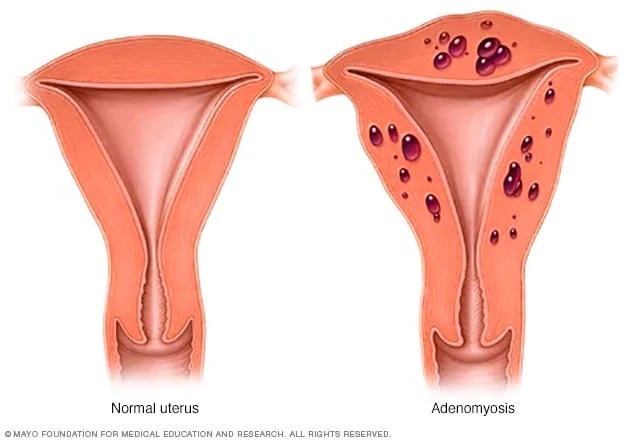
Then we have fibroids that start inside the uterus and can either project inwards or outwards. While they don’t technically grow outside the womb, as we’ll discuss shortly they can present externally by growing through the uterine wall.
What is Each Condition?
The obvious place to start is to explain what fibroids are, and what endometriosis and adenomyosis are.
Adenomyosis
Adenomyosis is a condition where the lining of the womb extends abnormally deep into the uterus. The uterine tissue and cells grow deep in the muscular wall of the uterus and thickens it. This is more common than previously thought (affecting up to 70% of women).
Endometriosis
Endometriosis is a disorder where tissues similar to the tissue that grows inside the uterus (the endometrium), grows outside the uterine cavity. It commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis.
When you have endometriosis, the endometrial-like tissue that is now growing outside your uterus still behaves like it would if it were inside your uterus - it thickens, breaks down and bleeds with each menstrual cycle. But instead of leaving your body, it becomes trapped in your pelvis.
Initially this isn’t a problem, but over time the tissue can become irritated, eventually leading to scar tissue and severe pain during periods. In some cases it can also cause issues with fertility.
Fibroids
Fibroids can grow in a single node (that is, by itself) or in a cluster. Most clusters vary in size between 1mm and 20cm in diameter. In some extreme cases, they can grow to the size of a watermelon.
Fibroids can distort the lining of the uterus, leading to heavy or abnormal bleeding, pelvic pain, and iron deficiency anemia. Very large fibroids can also put pressure on the surrounding organs, causing pain and bloating as well as bladder problems.
Symptoms
Adenomyosis
Sometimes, adenomyosis produces no signs or symptoms, or only mild discomfort. However, when it does present symptoms, adenomyosis can result in:
- Heavy or prolonged periods
- Severe cramping or sharp, knifelike pelvic pain during menstruation
- Chronic pelvic pain
- Painful intercourse
- Tenderness or swelling in your abdomen (which may indicate an enlarged uterus)
Endometriosis
- Painful periods
- Pelvic pain and cramping may begin before and extend several days into a menstrual period. You may also have lower back and abdominal pain
- Painful intercourse
- Pain with bowel movements or urination, usually during menstruation
- Excessive or heavy menstrual bleeding
- Infertility
- Other signs and symptoms such as fatigue, diarrhea, constipation, bloating or nausea, especially during menstrual periods.
Fibroids
- Heavy periods
- Passing large clots
- Tiredness
- Painful periods and/or sex
- Infertility
- A feeling of pressure in the pelvis
- Frequent urination and difficulty emptying the bladder
- Constipation
- Leg or back pain
- Incontinence
Causes
Adenomyosis
We don’t know for sure, but we know there is some link to endometriosis. Adenomyosis often co-exists with fibroids, and is routinely misdiagnosed as fibroids.
Despite this, some experts have developed a number of theories for what might cause adenomyosis:
- Tissue growth - some experts believe that endometrial cells, from the lining of the uterus, invade the muscle of the uterine walls.
- During development - some experts believe endometrial tissues ends up in the uterine muscle when the fetus is first formed.
- Childbirth - other experts believe a link exists between adenomyosis and childbirth, where inflammation of the uterine lining during postpartum periods can break the normal boundary of the cells that line the uterus.
- Stem cells - a recent theory proposes that bone marrow stem cells might invade the uterine muscle, causing adenomyosis.
Endometriosis
Once again, the exact cause is unknown, but some possible causes include:
- Retrograde menstruation. This is one of the oldest theories, and involves menstrual blood containing endometrial cells flowing back through the fallopian tubes and into the pelvic cavity instead of out of the body. These endometrial cells stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle.
- Hormones such as estrogen may transform embryonic cells (cells in early stages of development) into endometrial-like cells.
- After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
- The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of the body.
- A problem with the immune system may make the body unable to recognize and destroy endometrial-like tissue that's growing outside the uterus.
Fibroids
Despite extensive research, we still aren’t sure what causes fibroids to grow. Some common theories include:
- Family history – if your mother, sister, or grandmother have fibroids, you may have a higher risk
- Pregnancy – hormone changes during pregnancy can cause fibroids to develop and grow quickly
- Obesity – obesity is a risk factor for a wide variety of health conditions, and some studies have shown that an unhealthy weight may affect the development of uterine fibroids
- Blood pressure – having a higher than average blood pressure for your age has been shown to have a relationship to uterine fibroids.
- Age – women over age 40 are much more likely to develop fibroids.
- Diet – a diet high in red meat and alcohol and low in green vegetables, fruit, and dairy may increase the risk of developing fibroids, although this is yet to be conclusively proven.
- Early-onset of puberty – some studies have found that women who entered puberty at an earlier than average age have an increased chance of developing fibroids.
Diagnosis
Adenomyosis
Adenomyosis can be identified on transvaginal ultrasound but is often missed. An MRI of the pelvis is far more sensitive for detection of adenomyosis as well as allowing identification of all fibroids and other potential causes of symptoms such as endometriosis. Accurate diagnosis is important as this affects treatment options.
Endometriosis
- Physical exam - During a pelvic exam, your doctor will manually feel your abdomen for cysts or scars behind the uterus.
- Ultrasound - Your doctor may use a transvaginal ultrasound or an abdominal ultrasound. Your doctor will be able to see images of your reproductive organs and be able to identify cysts associated with endometriosis.
- MRI - An MRI is an exam that uses a magnetic field and radio waves to create detailed images of the organs and tissues within your body.
- Laparoscopy - The only certain method for identifying endometriosis is by viewing it directly. This is done by a minor surgical procedure known as a laparoscopy.
Fibroids
- Ultrasound – while ultrasounds are useful for detecting abnormal growths in the uterus, they often have trouble differentiating uterine fibroids from other gynecological conditions (such as adenomyosis, which can also be treated by UFE).
- MRI – MRI scans are used to give the full picture in regards to your uterine fibroids. This helps us to determine whether they’re best managed through medication, surgery, or embolisation.
- Hysteroscopy – this procedure uses a small camera to examine the inside of the uterus and look for abnormalities.
Treatment
Adenomyosis
- Anti-Inflammatory Medications - For mild cases, medication such as ibuprofen can be used to reduce blood flow during your period and relieve severe cramps.
- Hormonal Treatments - Hormonal treatments can help to control increased estrogen levels that may be contributing to your symptoms. Treatments include contraceptives, such as birth control pills.
- Endometrial Ablation - This involves removing or destroying the lining of the uterine cavity (the endometrium). This is not a suitable treatment for everyone since adenomyosis often invades deep into the muscle.
- Hysterectomy - A hysterectomy is the surgical removal of the uterus. It’s a major surgical intervention with serious side effects, and only suitable for women who don’t plan on having any more children.
- Uterine Artery Embolisation - This minimally invasive approach is almost identical to Uterine Fibroid Embolisation, performed for uterine fibroids. This allows significant symptom control in a majority of patients and can prevent the need for a hysterectomy. This procedure is performed by an Interventional Radiologist, is minimally invasive, and avoids scar tissue developing in the uterus.
Endometriosis
- Pain medication - anti-inflammatory medication such as ibuprofen can help relieve pain and other symptoms.
- Hormone treatment - hormone medication may slow down the growth of endometrial tissue and prevent new tissue growing. Hormone supplements aren’t a permanent solution.
- Laparoscopic surgery - a small incision is made in the abdomen, near your belly button, and a thin viewing instrument (laparoscope) is inserted to remove endometrial tissue. This can be done at the same time as checking for endometriosis.
- Hysterectomy - complete removal of the uterus will remove all endometrial tissue, but prevents future fertility. As such, many doctors are moving away from this option for treating endometriosis.
Fibroids
There are a number of treatment options available for fibroid sufferers. The first line of treatment is usually conservative management, such as pain control through medication. Many women find this to be effective in managing their symptoms, but it may not benefit all cases, particularly if fibroids are affecting your fertility, or if you have allergies to certain medications.
If medication fails, the size, location, and the number of fibroids are assessed to determine the next course of action, as well as your symptoms, menopausal status, and whether or not you wish to become pregnant in the future.
If it’s seen as in your best interest, it may be recommended that your fibroids be removed surgically (either by myomectomy or hysterectomy), or by uterine fibroid embolisation (UFE).